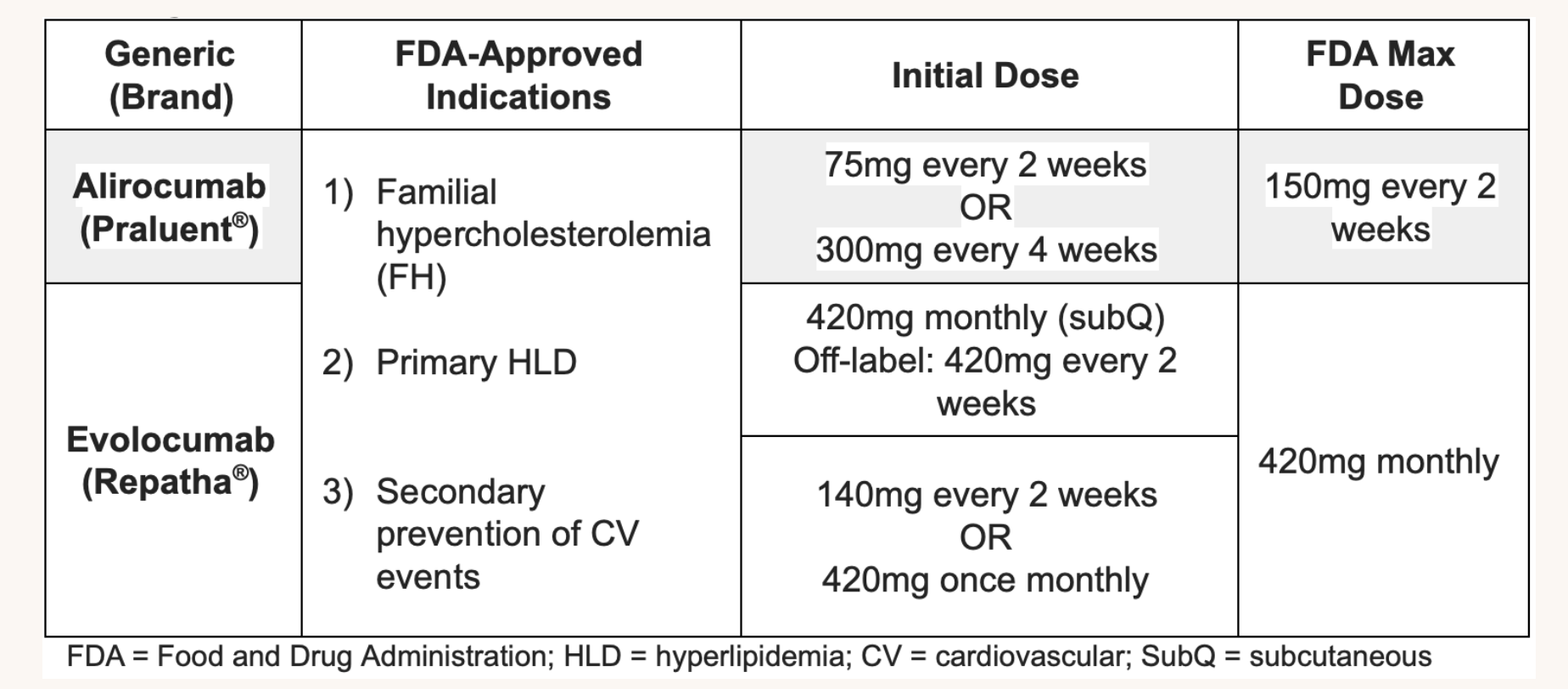
Lipid Therapy 2018 Guideline on the Management of Blood Cholesterol Elevated LDL-C Diet: Trans/Saturated Fats, Weight gain, Anorexia, Alcohol Drugs: Diuretics, Cyclosporines, Glucocorticoids, Amiodarone Diseases: Biliary Obstruction, Nephrotic Syndrome Other: Hypothyroidism, Obesity, Pregnancy Dietary fat has a greater impact on serum LDL-C than does dietary cholesterol intake Fats should be limited to ≤30% of total caloric intake Saturated fats should be limited to ≤10% of calories (7% if LDL-C above goal) Elevated Triglycerides 2021 ACC Guideline for the Management of ASCVD Risk Reduction in Patients With Persistent Hypertriglyceridemia Diet: Weight gain, Very low fat diets, High intake of refined carbs, Excessive Alcohol intake Drug: Oral estrogens, Glucocorticoids, Bile Acid Sequestrants, Protease inhibitors, Retinoic acid, Anabolic steroids, Sirolimus, Raloxifene, Tamoxifen, BB (not carvedilol), Thiazides Diseases: Nephrotic Syndrome, Chronic Renal Failure, Lipodystrophies Other: Poorly controlled diabetes, Hypothyroidism, Obesity, Pregnancy Higher-Risk The following factors that may be considered for the identification of higher-risk patients with clinical CV disease: - Age ≥65 years, prior MI or non-hemorrhagic stroke, current daily cigarette smoking, symptomatic PVD with prior MI or stroke, history of non-MI related coronary revascularization, residual coronary artery disease with ≥40% stenosis in ≥2 large vessels, HDL ≤40 mg/dL for men and ≤50 mg/dL for women, hs-CRP ≥2 mg/L, or metabolic syndrome Liver Statins (HMG-CoA reductase inhibitors, LDL) MOA: RLS in intracellular biosynthesis of cholesterol (competitive inhibition) Increases LDL receptors on liver cell membranes Remove circulating LDL and digest it Reduces serum w/ minimal liver LDL change Decrease CoQ10 synthesis (ubiquinone) Statins metabolized by CYP450 3A4 Lovastatin, simvastatin, atorvastatin Benefits Plaque stabilization Inflammation Reduction, decrease CRP Improve endothelial function Decreased Thrombogenicity Potency: High Potency: lower LDL by ≥50% Large LDL Decrease (20-60%, 1st line) Doubling dose adds 6% effect Rosuvastatin (Crestor) High: 20-40mg Moderate: 5-10mg CKD ≥3 or Dialysis: 10mg Can be used in Cirrhosis Atorvastatin (Lipitor) High: 40-80mg Moderate: 10-20mg CKD ≥3 or Dialysis: 20mg Lipophilic, not renally cleared Simvastatin (Zocor) Moderate: 20-40mg Low: 10mg CKD ≥3 or Dialysis: 20mg Lipophilic, not renally cleared Pravastatin (Pravachol) Moderate: 40-80mg Low: 10-20mg CKD ≥3 or Dialysis: 40mg Least muscle SE, preferred in elevated LFTs Not renally cleared, can be used in Cirrhosis Lovastatin (Mevachor) Moderate: 40mg Low: 20mg CKD ≥3 or Dialysis: Not evaluated Lipophilic Fluvastatin Moderate: 80mg Low: 20-40mg CKD ≥3 or Dialysis: 80mg Least muscle SE, not renally cleared Pitavastatin Moderate: 2-4mg Low: 1mg CKD ≥3 or Dialysis: 2mg Most effective, first line to lower cholesterol and LDL Moderate HDL increase Moderate Triglyceride Decrease Trials IMPROVE-IT (2015) Adding ezetimibe to statin further reduces CV events in the population, suggesting the maximal LDL reduction is the key mech SE: Hepatotoxicity If AST/ALT ≥ 3x ULN, reduce or switch Myalgias (symmetrical proximal muscle weakness or tenderness) Myositis/Myopathy Rhabdomyolysis 1%, CK ≥ 10x ULN + Renal injury Statin-associated autoimmune myopathy (HMGCR antibodies) High Intensity Renal Dysfunction More common w/Rosuvastatin/Simvastatin Proteinuria, Hematuria, AKI Switch to Atorvastatin, Fluvastatin, Pravastatin Diabetes Mellitus Increased plasma glucose concentrations CI: Pregnancy, Lactation, Acute liver failure/decompensated cirrhosis VATER association, TE fistulas, anal atresias Interactions Amlodipine, diltiazem, verapamil + either simvastatin or lovastatin increases risk of toxicity Gemfibrozil: Increased risk for muscle toxicity Colestipol and antacids decrease plasma concentration Amiodarone, cranberry, grapefruit Monitoring Lipid profile at baseline, then 6-8 weeks after LFTs and TSH at baseline, ± CK level Niacin Drugs: Niacin Lipolysis Decreased in Adipose Tissues Moderate LDL Decrease Large HDL Increase Moderate Triglycerides Decrease Flushing and pruritis is caused by prostaglandin-induced peripheral vasodilation Low dose aspirin may reduce symptoms Lomitapide (Juxtapid) Mitratapide (Yarvitan) GI Tract Ezetimibe (Zetia) Cholesterol Absorption Inhibitor at Intestinal Border, NPC1L1 Moderate LDL Decrease (15-20%, 2nd line) May be used in ASCVD w/very high risk on max statin with LDL ≥70 or non-HDL ≥100 HDL Unchanged Triglycerides Unchanged Bile Acid Sequestrants/Resins (LDL) Drugs: Cholestyramine, Colesevelam (Welchol), Colestipol Inhibits reabsorption of bile acids, decreasing lipoprotein levels Alone or in combo with Stains Moderate LDL Decrease Mild HDL Increase Triglycerides Unchanged-Increased Blood Vessels Fibrates (Lipoprotein lipolysis Induction, PPAR) Drugs: Fenofibrate (Tricor), Gemfibrozil (Lopid) Not as favorable CV effects as statins or niacin Moderate LDL Decrease Moderate HDL Increase Large Triglycerides Decrease (35-50%) PCSK9 Inhibitors (LDL) MOA: Proprotein convertase subtilisin/kexin type 9 (PCSK9), produced by liver that leads to degradation of hepatocyte LDL receptors via internalization and destruction Evolocamab (Repatha) Alirocumab (Praluent) Indications High Risk 40-75 + Baseline LDL ≥190 and who do not achieve 50% reduction in LDL or LDL <100 on max stat and ezetimibe Decrease LDL-c by 60% Decrease TGs by 10-15% HDL increase by 5-10% Lp(a) decreased by 25-30% Trials FOURIER (2017) Among patients with clinical atherosclerotic disease and LDL ≥ 70 despite high or moderate intensity statin therapy (70% high intensity), Evolocumab resulted in an absolute 1.5% reduction in MACE at 26 months Mainly from reduction in nonfatal MI, stroke, and revascularization No mortality benefits Absolute reduction in CVE was greater with more advanced CKD ODESSEY OUTCOMES (2021) In recent ACS and LDL ~70 on optimized statin therapy, PCSK9 inhibitors provide clinical benefit only when lp(a) is at least mildly elevated. Mortality benefit in the long term SE: Injection site reaction Resources
Lipids Statins